Fire has almost disappeared as a cause of death in the developed world. A similar approach could do the same for infectious diseases.
In November 1977, a smallpox eradication team descended on the Somalian port city of Merca. They vaccinated 54,777 people in two weeks, going house to house and setting up checkpoints to vaccinate everyone entering and leaving the city. It had been ten years since the World Health Organization had made a fresh commitment to end the pandemic, and by 1976 Somalia was the last country with cases still being detected.
The vaccinators’ mission was in response to the case of Ali Maow Maalin, a 23-year-old hospital cook who had the misfortune of spending a short car journey accompanying two children infected with smallpox. Having been asked for directions – and not realizing the danger he was in – he got in the car to provide help. The ride was no longer than 15 minutes, so his fleeting exposure was missed by the contact tracers. Ten days later he got sick. Had he been immediately identified and vaccinated, the outbreak could have ended with those two children.
Subscribe for $100 to receive six beautiful issues per year.
Despite that unfortunate misstep, his case eventually got the attention of the local smallpox eradication team, which sprang into action. The initial vaccination campaign wrapped up in a few weeks, and precautionary house-to-house searches in Merca that continued into 1979 turned up no further cases. In May 1980, the 33rd World Health Assembly officially declared smallpox eradicated. The smallpox pandemic, which had ravaged the world for centuries, ended with Maalin.
Smallpox remains to this day only one of two infectious diseases to have been intentionally eradicated from nature, and the only one that infects humans. The existence of the virus is preserved only in lab samples, such as the one that claimed smallpox’s last victim, and in the knowledge of its genetic code.
As it turns out, smallpox had a number of features that made eradication through vaccination more feasible than for most other infectious diseases. It was a human disease with no animal reservoir. Symptoms were distinctive, with no asymptomatic transmission. Smallpox’s genome is made of DNA, which means it has a much slower mutation rate than many other viruses. Most natural diseases of pandemic potential have one or more of these crucial differences. And that’s before we take seriously the potential properties of unnatural pandemic diseases, made possible through advancing the frontiers of synthetic biology.
The eradication of smallpox ranks among humanity’s greatest triumphs, and the last push by the WHO cost only about one billion dollars in today’s currency. But if we want to eliminate the risk of future pandemics we need to look elsewhere for inspiration.
We can find more instructive lessons in another terrifying force of nature. Like infectious disease, it has been with us since the dawn of our species. It can start small and quickly grow exponentially out of control. It too became a bigger threat as civilization advanced, and to this day it profoundly shapes how we live and work.
The gift of Prometheus
Boston, 1760. New York City, 1776. New Orleans, 1788. New Orleans, 1794. New York City, 1835. New York City, 1845. Pittsburgh, 1845. Toronto, 1849. Montreal, 1852. Portland, 1866. Chicago, 1871. Boston, 1872. Vancouver, 1886. Baltimore, 1904. Toronto, 1904. All of these are events in North American history that have the name Great Fire.
The rapidly industrializing and urbanizing United States chose timber as a cheap building material, which made the North America of the late eighteenth and nineteenth century especially susceptible to large city fires. But the major urban conflagration was hardly a uniquely North American phenomenon. Numerous European cities burned down several times; Tokyo and its antecedents suffered from a number of great conflagrations; Nero apocryphally fiddled while Rome burned in 64 AD, and the destruction of the Great Fire of London in 1666 led to the invention of private fire insurance, as well as the first organized systems of fire protection provided by those same insurance companies.
All of these fires destroyed large portions of cities, and in some cases almost all structures. It’s often remarked that cities were death traps of disease until advances in sanitation and medicine. But how frequently they went up in flames is less remarked on.
The total cost of fire today in the United States is estimated to be in the order of two percent of GDP, but that’s not because there is still a lot of fire. Actual losses due to fire constitute only 17 percent of that total, of which the vast majority is the statistical cost of death and injuries translated into dollars (in this particular estimate, the value of a statistical life is $9.6 million).
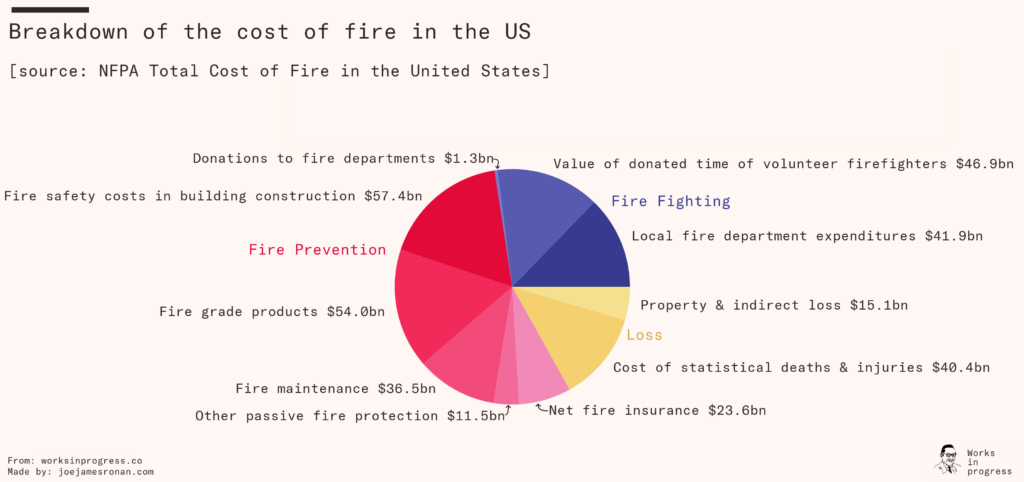
The remaining 83 percent constitutes the cost of fire protection and prevention, representing $273 billion in 2014. Of that, only $40 billion is the direct cost of fire departments. By far more of the expenditure is on indirect fire protection and prevention, like making buildings and products firesafe. These are crude high-level estimates (for example, the cost of making nonresidential buildings firesafe is assumed to be construction expenditure times 12 percent). But to give you a sense of scale – this is like funding an entire Apollo lunar program (estimated total cost about $280 billion in today’s dollars) every single year.
But it’s worth it, because the cities used to burn.
What if fire, but worse
Unless you worked in a hospital or a care home, the destruction of Covid-19 was something that mostly happened out of sight, our griefs observed in private. We viscerally experienced the disruption caused by trying to slow it down, but unlike fire it is a natural force that we cannot see, hear, or touch. Pandemics are less dramatic, less cinematic, than fire.
The deadliest fire in US history – triggered by the 1906 San Francisco earthquake – killed around 3,000 people. If we look at all civilian deaths from fire between 1977 and 2020, approximately 200,000 people died in the United States. Restricting the comparison solely to deaths within the United States, the Covid-19 pandemic is around 350 times worse than the worst ever fire, and 5 times worse than all fires in the last 45 years combined. The total cost of the Covid-19 pandemic is estimated to be in the order of $16 trillion in the US alone – this would represent about 50 years’ worth of the equivalent estimated annual cost of fire. Since the beginning of the twentieth century, there have been no fewer than five pandemics that are estimated to have killed 100,000 people or more in the United States alone (three Influenza pandemics, Covid-19, and HIV/AIDS). It was worth taming the great urban conflagration, and it will be worth taming pandemics.
We can categorize strategies to mitigate the risk of the fire into four approaches: prevention, detection, passive protection, and active protection. In the same way that managing fire risk is not all (or even primarily) about more firefighters and fire engines, managing the risks of pandemics will require a suite of different strategies over and beyond developing new pharmaceuticals.
Active protection
There are three ingredients of combustion – oxygen, heat, and fuel. Fire suppression technologies act by either physically or chemically denying a fire one or more of those ingredients. While classification systems vary, for most purposes the four broad types of fire – ordinary combustibles, flammable liquids and gases, metal, and electrical – have different physical and chemical properties that can require different technologies or techniques to extinguish. For example, the early twentieth century saw the invention of chemical foam and carbon dioxide fire extinguishers, which for the first time allowed for the effective suppression of flammable-liquid fires.
Biology is less kind to us than chemistry. There are approximately 26 families of viruses that are known to infect humans, and the differences between families matter just as the differences between the classes of fire matter. Different viruses infect different cells through different means, though viruses within the same family share structural features that mean knowing how to combat one can help you with the others, and some pharmaceuticals are effective across different viruses within a family.
Take the current monkeypox outbreak as an example. We have two pharmaceuticals being used against the disease – the Jynneos vaccine and the antiviral tecovirimat – that were originally developed to guard against a potential smallpox attack by bioterrorists. Another example would be very familiar: Every year when you get a flu shot, you get a different formulation to protect you from the strains that are expected to dominate the year’s flu season – but the underlying technology and production method is often the same.
As for Covid-19, one of the crucial pieces of the vaccine puzzle was to ensure that the key antigen our immune system learned to respond to – the coronavirus spike protein – was encountered by our immune system in the shape it would have before it unlocked the door into our cells. This prefusion spike protein was discovered when designing a vaccine for another coronavirus, Middle Eastern respiratory syndrome (MERS), and scientists learned how to re-create it for the Covid-19 vaccine. Had that research not already been done before the pandemic started, we would have waited longer for effective vaccines.
For around half of the virus families that infect humans, we do not have a licensed vaccine for any virus within the family. If we are to mimic our success in fighting fires with different types of extinguishers, then this must be the starting point. We should also be using a prototype pathogen approach to develop antivirals and monoclonal antibodies for at least one virus within each family, as well as aiming to develop broad-spectrum vaccines and monoclonal antibodies for entire virus families and broad-spectrum antivirals that are effective across multiple families. We can also accelerate the development and authorization timeline for monoclonal antibodies, learning lessons from the expedited regulatory pathway of mRNA vaccines in the Covid-19 pandemic.
But just as fire suppression is most effective the earlier the fire and type of fire is identified, to respond to a novel pathogen effectively we need to know what we’re facing. And the faster we know that, the easier and less costly it will be to contain the next pandemic.
Detection
Fire alarms reduce the time it takes a fire to be reported by an average of around 20 minutes in the United States. To put that number in context, in the UK it takes on average seven to eight minutes for emergency services to respond to a fire, and in the USA the target for fire departments is to respond to 90 percent of incidents with the first engine in just over five minutes.
Think about how much effort and planning goes into achieving rapid fire department response times. It’s not just the training of the call handlers and the firefighters themselves, who must be prepared to act with ruthless efficiency at a moment’s notice. Locations of fire stations, the ability to preempt traffic signals, regulations of access roads – all these things and many more contribute to the continued effort to shave seconds off response times. But all that effort pales in significance when compared to how easily we can start the response earlier, before a fire grows exponentially out of control.
It is therefore not surprising that a 2016 meta-analysis found that the risk of fire death is halved by having smoke alarms in the house, and a Canadian study concluded alarms reduce the risk of a fire spreading beyond room of origin by 71 percent.
The first complete genomic sequence for SARS-CoV-2 was posted on the website virological.org on 10th January 2020. The next day, authorities in Wuhan reported the first death. It is currently thought that the virus started circulating about two to three months earlier. It’s easy for our intuitions about exponential growth to be wrong, so to illustrate the importance of this time: A virus that infects double the number of people every week will be infecting a thousand times more people every day after ten weeks of exponential growth. If infections double every 2.5 days, as is estimated to have occurred for SARS-CoV-2 infections in Hubei province in January–February 2020, one new infection per day would become millions in less than two months. We need a better fire alarm system for pandemics, because it is far easier to contain a threat early on.
It is relatively cheap to test for viruses when you already know what you are looking for – the PCR tests that we have all used to test ourselves for Covid-19 detect genetic sequences by amplifying them if they are already in the sample. But you need a known gene sequence target called a template in order to do a PCR test at all. While we should absolutely be working to make targeted testing cheaper and more ubiquitous, it won’t detect a new threat.
This approach needs to be complemented with target-agnostic next-generation metagenomic sequencing, which attempts to read every single piece of genomic material within a sample that could include many different kinds of biological material. You don’t just sequence one target within a sample that you know you want, you sequence everything. With systematic metagenomic sequencing of environmental samples it could be possible to look beyond hospitals as the first point of contact with a novel pathogen and identify biological threats before someone even gets sick enough to seek urgent medical care. However, while such a system is theoretically possible at the current state of technology the quantity of sequencing would be prohibitively expensive. Furthermore, we also don’t yet know how we would analyze the vast amount of data such an early-warning system would create. The analytical aspect of this challenge is currently being taken on by the Nucleic Acid Observatory based at the MIT Media Lab.
We should not understate the technical challenges of developing such a global alarm system, but we are already failing to make the most of the technology that is already available to us. For example, poliovirus is being found in wastewater across the world using PCR techniques, and has almost certainly been there for some time before we decided to look for it. In New York, they only started looking after the first case of paralysis in an unvaccinated patient.
We don’t have all the tools in the tool kit that we would like yet. But creating systematic early-warning systems with the technologies that we have available today – including existing wastewater and clinical tools – will not only have a public health benefit. It will give us the opportunity to develop operational infrastructure for sample collection and storage to which new sequencing techniques and analytics can be applied in the future. And it can lay the groundwork for global institutions for coordination and information sharing that will become even more powerful once other forms of environmental sampling and metagenomic sequencing become feasible.
Passive protection
Fires are still common occurrences, with fire departments responding to about 1,000 home structure fires every day in the USA, but they very rarely spread to adjacent structures. That’s not just because the alarm is sounded, automatic sprinkler systems are engaged, and firefighters equipped with modern fire suppression equipment quickly arrive at the scene. We have engineered the whole urban environment around preventing the spread of fire.
Regulations of building materials because of fire have been around for many centuries. In the thirteenth century, the city of Lübeck, in Germany, restricted the use of wood in construction as a response to the second devastating fire in a hundred years. The spread of the Great Fire of Boston in 1872 was blamed on wooden roofs, known as mansards, that topped the otherwise brick buildings and were an architectural fad of the time. As well as banning certain materials in construction, there are a litany of different codes and regulations around fire hydrants, unprotected vertical openings, void spaces, and concealed spaces.
Regulation of building construction can be costly and unpopular. After the Great Fire of Chicago in 1871, proposed restrictions on the use of wood in construction were materially watered down due to opposition from working-class constituencies that did not want to see the cost of new homes rise. Notwithstanding these real costs, failure to appropriately supervise and enforce regulations of building materials can end in tragedy like the 72 lives lost in the Grenfell Tower fire. The remedial cost of retrofitting buildings in the UK clad with similarly inappropriate material is expected to run into the billions of pounds.
We now use firewall as a metaphor, but its original meaning is a wall that is designed to prevent the spread of fire. The fire insurance industry had a very strong incentive to lobby for building code regulations that would contain fires; but compartmentalizing fire between structures is much more lucrative from an insurance standpoint relative to within. A number of famous single-building fires resulted in larger loss of life than the urban conflagrations that preceded them – 146 dead in the Triangle Shirtwaist Factory fire of 1911, 119 dead in the Winecoff Hotel fire of 1946 – and these were in buildings that were ostensibly firesafe. They were only safe if you were outside the building when the fire started. Containment of fire within structures, as well as minimizing loss of life through ensuring appropriate means of escape, came more slowly.
This reduction in the spread of fire has been nothing short of transformational, not just a difference in quantity but in kind. And this is an area where I see the biggest case for optimism when it comes to infectious disease.
We already know that existing HEPA filters are capable of removing SARS-CoV-2 from indoor air on a hospital ward and ventilation is extremely effective at reducing transmission of airborne pathogens. It is a no-brainer to fund trials of implementing more and better air filtration and ventilation systems in high-risk buildings. Even outside of pandemics, hospital-acquired or nosocomial infections are a significant burden on health care systems, with estimates of the proportion that are airborne in the region of ten percent. Reducing these non-pandemic infections alone could be worth billions of dollars in both direct cost saved and the statistical value of human lives. And it can potentially be done with existing technology and at reasonable cost.
But there is also an emerging technology that could complement air filtration and potentially transform microbial suppression in the built environment. UVC light is a potent antimicrobial with a long history of specialized use, but its main limitation is that UVC lightwaves with a wavelength over 235 nanometers penetrate our skin through to the DNA in our cells and can cause cancer.
However, UVC with a wavelength below 235 nanometers is readily absorbed by even a small layer of protein. The photons are therefore blocked from reaching and degrading our DNA by absorption in the outer layer of human skin that consists of dead cells. This shorter wavelength far-UVC is still very effective against airborne microbes – or indeed any other nucleic acids that remain exposed to the far-UVC photons – and all studies so far show these wavelengths to be safe.
We shouldn’t overhype new technologies, and there are many challenges to overcome and questions to answer. For example, we need to do more testing on the effect of far-UVC on the common materials, cosmetics, and surfaces it would come into contact with if deployed ubiquitously, and how its efficacy interacts with existing ventilation systems. While it has shown much promise against small virus particles suspended in the air (such as coronaviruses), how effective it will be for diseases spread by larger respiratory droplets requires further investigation. We need to do more safety studies to make sure that the sources of far-UVC we deploy don’t emit wavelengths over 235 nanometers as a by-product. Most studies have been done at a wavelength of 222 nanometers, and there may be trade-offs of different sub-235-nanometer wavelengths that we have yet to explore. And with an ambitious vision of ubiquitous deployment, we need to test realistic edge cases such as how safe it is if you have an open wound. There is a lot to do in order to bring far-UVC out of the lab and into our public spaces. But it is the most promising new candidate for building a pandemic firewall.
More prosaically, we can also wear a firewall on our person. Personal protective equipment (PPE) can range from cheap reusable face masks of varying levels of comfort and effectiveness all the way to cumbersome full body suits for those in most danger of exposure to deadly pathogens. But current PPE is lacking in almost every dimension. It is uncomfortable, unattractive, impractical, insufficiently reusable, and imperfectly protective. We can and need to do better.
Next-gen PPE could involve innovations in multiple disciplines such as materials, design, and engineering. We need to safeguard the wearer with as minimal burden as possible, and add features such as the ability to neutralize pathogens (for example, incorporating naturally antimicrobial materials such as copper) and detect potential exposures. Stockpiling in advance can have an outsize impact if an outbreak can be suppressed before becoming a pandemic. However, if early suppression of an outbreak is unsuccessful we also have to ensure that PPE can be rapidly produced from widely available materials. While there could be intermediate commercial applications of next-gen PPE in health care settings and for the severely immunocompromised, it is unlikely that the investment required will happen without significant public sector and philanthropic support. One option could be making advanced commitments to purchasing PPE that meets design specs, as has been pioneered in vaccines.
It is underappreciated how fortunate we were that essential services and supply chains broadly continued to function during the Covid-19 pandemic, something I saw firsthand managing the team responsible for the supply of fresh fruit at the UK’s second-largest supermarket. Had more extreme social distancing to suppress transmission been necessary, this would have threatened numerous critical points in the supply chain such as packing facilities, transportation, and warehouses, as well as essential retail stores themselves. In such a scenario, we would have had an unenviable choice between uncontrolled spread of disease and losing the foundations of modern civilization – not only mass production and distribution of goods, but also energy, transportation, and medical services. And it is optimistic to think this would even be a choice; individual workers can vote with their feet if their lives and those of their families are put at excessive risk by showing up to work.
SARS-CoV-2 is not nearly as infectious as measles, as virulent as SARS-CoV-1, or as deadly to young children relative to older adults as influenza. But if any of those things had been different, we would have been in big trouble.
Passive protection measures such as ventilation, far-UVC light, and next-gen PPE will mean less social distancing is required to control the spread of a pathogen, and make society resilient to much more transmissible and deadlier viruses than SARS-CoV-2. They will be essential were we to encounter a pathogen that is as hard to vaccinate against as HIV has proven to be, or spreads as silently as HIV did before it started causing AIDS.
Prevention
The number one cause of fire is human behavior. When that behavior is deliberate, we call it arson. But for the most part, the fire risks we create come from the innocent – if occasionally negligent – pursuit of work and play. By far the leading cause of home fires in the US is cooking, and the main factor for cooking fires is leaving equipment unattended. More than one quarter of those who died from cooking fires were sleeping at the time. And it’s not just home fires; the Great Fire of London itself began in a bakery on Pudding Lane.
In a world of comprehensive fire protection and detection, engaging in unsafe fire behaviors does not imperil whole cities. Thankfully, we don’t need to call for the restriction of deep fat fryers because of the risk of causing hundreds of billions of dollars’ worth of damage. But were the great urban conflagration still a realistic possibility, the need for responsibility would be far more urgent and our risk tolerance far lower.
One of the most concerning natural pathogens of pandemic potential that we are already aware of is H5N1 Influenza A, a form of bird flu with a fatality rate in excess of 50 percent among identified cases. So far, infections have been rare as the virus does not efficiently transmit between humans – it’s usually only acquired by people who have had close contact with infected animals. But it remains a serious threat to global health – just this year tens of millions of chickens and other birds have been culled due to outbreaks of the disease.
A reasonable question one might ask is – how likely is it that this dangerous pathogen evolves the capability for human-to-human transmission? Researchers set out to try to answer exactly that through experimentation. They used what is called an animal model to study H5N1 – these are animals that either naturally or through genetic modification share relevant common features with humans for infection with the disease in question. In this instance, the animals were ferrets.
The research was successful, and a weakened form of H5N1 that was ferret-to-ferret transmissible was created – something the wild virus was not capable of doing. This type of research is often referred to as gain of function, although the term is imprecise, as deliberately manipulating biological entities to give them new properties can be totally innocuous (for example, inducing production of green fluorescent protein to make things glow is a common research technique). What we need to be concerned with is adding potentially dangerous functions, or what the NIH refers to as enhanced potential pandemic pathogens (ePPP). It falls under the larger umbrella of dual-use research of concern: research or technology that has the potential to do harm as well as good.
Advocates for conducting this research and publishing it in full will say that we learned something valuable: Evolution of H5N1 toward transmission in ferrets – which are a useful model for humans – is possible and now we know some of the possible changes to the virus that could make it happen. Detractors say: Not only are the benefits of this knowledge speculative, but you did this by actually creating a virus that could potentially transmit between humans. It’s a bit like doing a fire drill with an actual fire – maybe that is a better drill, but does the risk justify the reward?
While the evidence seems to point away from the theory that the source of the Covid-19 pandemic was the Wuhan Institute of Virology (WIV), the idea that a pandemic could occur as a result of an accidental breach of a high-containment laboratory is scientifically credible. Lab leaks have plenty of precedent, even from the highest-grade “BSL-4” labs. For example, the 2007 foot-and-mouth disease (FMD) outbreak in the United Kingdom was the result of a leaky waste pipe at the joint site of a BSL-4 lab and a vaccine manufacturer. Even more worryingly, shortly after the vaccine site was relicensed for production, FMD virus leaked again into the site drainage system. Fortunately it wasn’t released into the nearby environment, thanks to upgrades made to the drainage in response to the first leak, but it illustrates the challenges of maintaining biosecurity even when you are on heightened alert.
And even if the origin of SARS-CoV-2 was not the WIV, we have probably already had the first pandemic in humans caused by escape from a lab. The 1977 Russian flu pandemic is so genetically similar to ancestral H1N1 flu strains in the context of the normal mutation rate of influenza viruses that a lab sample is the most plausible origin.
Unfortunately, the risks of nature and well-intentioned research are not the only ones we need to be concerned about. While a virus of natural or benign origin is the most likely source of the next pandemic, there are greater dangers that we face. We also need to worry about biological arson.
Proliferation
States and terrorist organizations have attempted to harness biology as a weapon of mass destruction, and continue to do so. While I am much more confident that we will continue to see natural pandemics rather than deliberately engineered pathogens, the latter have the potential to be far deadlier. This possibility does not require great stretches of the imagination, as mass civilian death from a bioweapons facility accident has already happened at least once. In 1979, accidental release of weaponized anthrax spores from a Soviet plant is estimated to have killed at least 66 people. Fortunately anthrax is not contagious, which vastly limited the damage that this event could have caused. But an accidental (or, god forbid, deliberate) release of an engineered virus ranks up there with some of the very worst threats we could face as a species.
When it comes to weapons of mass destruction, states generally have the capacity to do things when they decide it is in their interest. In the domain of nuclear weapons, many of the arms control successes have been about shaping state intent – making it unattractive to pursue nuclear weapons rather than physically impossible. Where the perceived benefits outweigh the costs, they will just do it, as North Korea has done despite being a desperately poor country with low state capacity.
There is an analogue to the Nuclear Non-Proliferation Treaty, the Biological Weapons Convention (BWC), to which there are 183 signatories, including all major powers. However, it lacks enforcement capability and has far less institutional, political, and financial support behind it than the international regimes we have in place to monitor nuclear and chemical weapons development. To give you a sense of scale, the BWC is run on a budget smaller than that of a single McDonald’s restaurant.
The Soviet Union was also a signatory to the BWC, but we now know that despite this they secretly continued a vast biological weapons program in flagrant contravention of international law and human decency. The extent to which such programs continue in the Russian Federation – or any other country – is impossible to know for sure.
But in the short term, the most concerning trend is proliferation in the capabilities of non-state actors. Thanks to the increasing ubiquity of DNA synthesis technology, the people in the world who could be capable of assembling an influenza virus based on publicly available genetic sequences number in the tens of thousands. In an act that might plausibly have caused more harm than good, researchers proved that they could reconstitute horsepox – an extinct virus similar to smallpox – for a mere $100,000.
We cannot reasonably expect to reliably shape the intent of every single individual who might ever be capable of doing this work, especially as the bioeconomy grows. If it became possible for individuals to order highly enriched uranium online, I think we would all agree that this would constitute a threat to global security. We need to constrain the capability of non-state actors to do the biological equivalent.
At present, providers of synthetic DNA are not legally required to screen for dangerous sequences, though many do so voluntarily. A few organizations have risen to the challenge of ensuring synthesis providers have access to effective screening. One, the Nuclear Threat Initiative, a nonprofit whose focus is global nuclear and biosecurity, is in the process of launching the International Biosecurity and Biosafety Initiative for Science (IBBIS), an organization whose mission includes preventing the misuse of DNA synthesis technology. Separately, the Secure DNA Project aims to provide companies all over the world with free, fast, and secure screening of synthetic DNA orders.
We are fortunate that a small group of companies, nonprofits, altruistic scientists, and philanthropists are stepping in to help keep us safe. But while such efforts show promise, it remains to be seen whether they will successfully accelerate the universalization of synthesis screening. While we live in a time characterized with the return of Great Power conflict, we can take inspiration from the past that cooperation to reduce the threat of species-level catastrophe can and must take place even while we fight.
The will to act
The author of the first textbook on firefighting in English, James Braidwood, died in the line of duty while attending to the Tooley Street warehouse fire of 1861 in London. He preached a highly aggressive approach to firefighting, entering the building to attack what he called the seat of the fire. He was killed by a collapsing wall, a structural failure that would now be far less likely to happen under modern building regulations.
Braidwood wasn’t wrong about the most effective way of manually fighting a fire, which involves a lot of the bravery for which firefighters are rightly famous. But we didn’t solve the Great Fire through more and braver firefighters. The transformational change in fire safety we have seen in the 160 years since Braidwood’s death came from the efforts of innovators, engineers, campaigners, regulators, and legislators. It came from the deployment of new technologies to suppress fire, detect it quickly, and to prevent its spread. And it came from having the will to act, deciding that enough is enough and that we must use our talents and our money and our laws to ensure that it never happens again.
The pandemic prevention strategies in this article are inspired by the Apollo Program for Biodefense, a bipartisan initiative that the United States government recently came tantalizingly close to embarking upon. The American Pandemic Preparedness plan proposed last year by the Biden administration would authorize $88.2 billion over five years to pursue many of the projects and ideas you have just read about. With that total representing less than one percent of the costs of the Covid-19 pandemic, it’s not nearly enough. But it would have been a start.
Congress did not take up the call.
The White House has not given up, and we have a new window of opportunity right now with the recent release of the National Biodefense Strategy and Implementation Plan. It is the most ambitious and clearest plan yet that assigns actions to the relevant agencies tat can bring this vision of pandemic prevention closer to reality. The newly divided Congress does not make getting this done any easier, but the challenge remains no less important or urgent than it was before 9th November.
In every corner of the world, countless people have lost loved ones and made sacrifices to keep themselves and others safe. They have been through hell and they kept on going. Never in the existence of our species have so many people been on the front line in the fight against infectious disease, and it is within our ability to make all that loss and sacrifice mean something more.
How many more biological Great Fires do we need in order to act?
As for Ali Maow Maalin, he fully recovered from smallpox and later went on to work in the campaign to eradicate polio from Somalia. One of the children who was in the car with him, a six-year-old girl named Habiba Nur Ali, was not so lucky. She became the last person to lose her life to a wild smallpox infection.
In 2013, polio reemerged in Somalia. Ali was playing a key role in the response, carrying out vaccinations in his hometown of Merca, when he developed a sudden fever. Days later he was in the hospital, where he later died of malaria.
The end of pandemics will not look like the end of smallpox. There will never be a last outbreak of a disease of pandemic potential, just as there will never be a last fire. There will never be a last victim, or a single moment of celebration where we can say: We did it. This is not why I tell you the story of Ali Maow Maalin.
Ali unexpectedly found himself at a hinge of human history, a passenger at the end of a battle against one of the deadliest killers the world has ever known. He could have just thought himself fortunate to have survived and gone on to live an ordinary life. But that’s not what Ali did. He stepped up and carried on the fight to the next frontier. He had the will to act.
The question we have to ask ourselves is – do we?