We disinfect water before we drink it. Germicidal ultraviolet could make airborne disease as rare as those carried by water.
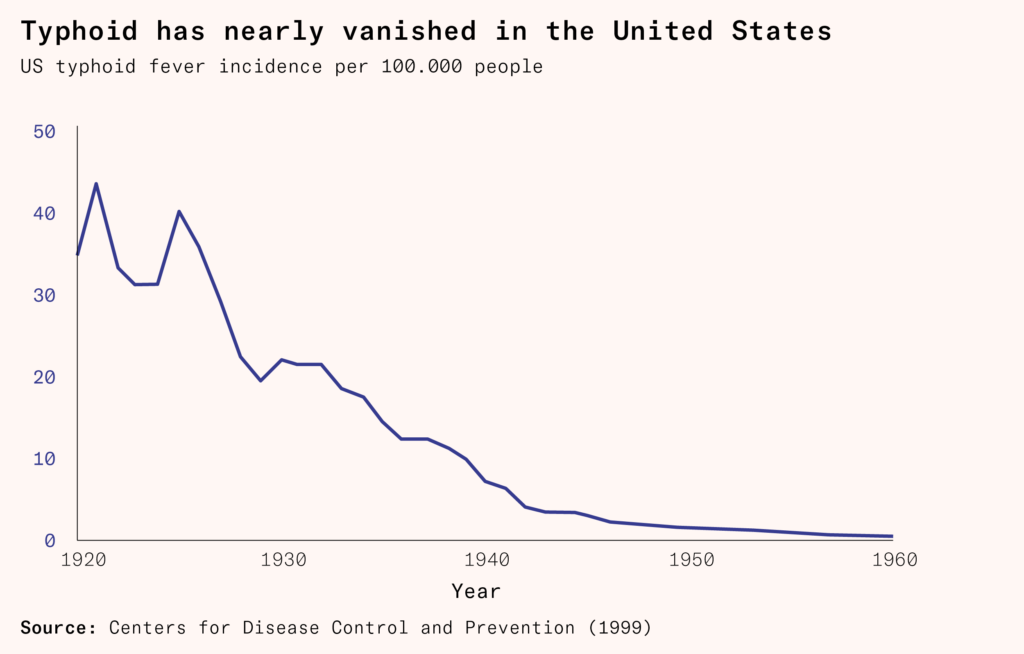
Between the 1860s and 1920, successive outbreaks of typhoid fever killed over 300,000 Americans. As population growth surged and people moved to urban areas en masse, American cities began to dump sewage in the same rivers that provided their drinking water. After epidemiologists linked typhoid outbreaks to water cleanliness, cities began building large-scale sand filtration systems in the 1890s, and in 1908, Jersey City pioneered the first continuous chlorination of a public water supply. By the 1920s, typhoid deaths had fallen by two-thirds, and waterborne diseases were in retreat across the country.
While typhoid and other waterborne diseases triggered vast engineering and regulatory responses, the equivalent airborne threats have not. Tuberculosis alone kills more than a million people every year around the world, yet the air in schools, clinics, and public buildings remains largely unfiltered and unmonitored. Covid-19, which killed over seven million people, demonstrated how rapidly airborne pathogens can spread in poorly ventilated spaces.
Subscribe for $100 to receive six beautiful issues per year.
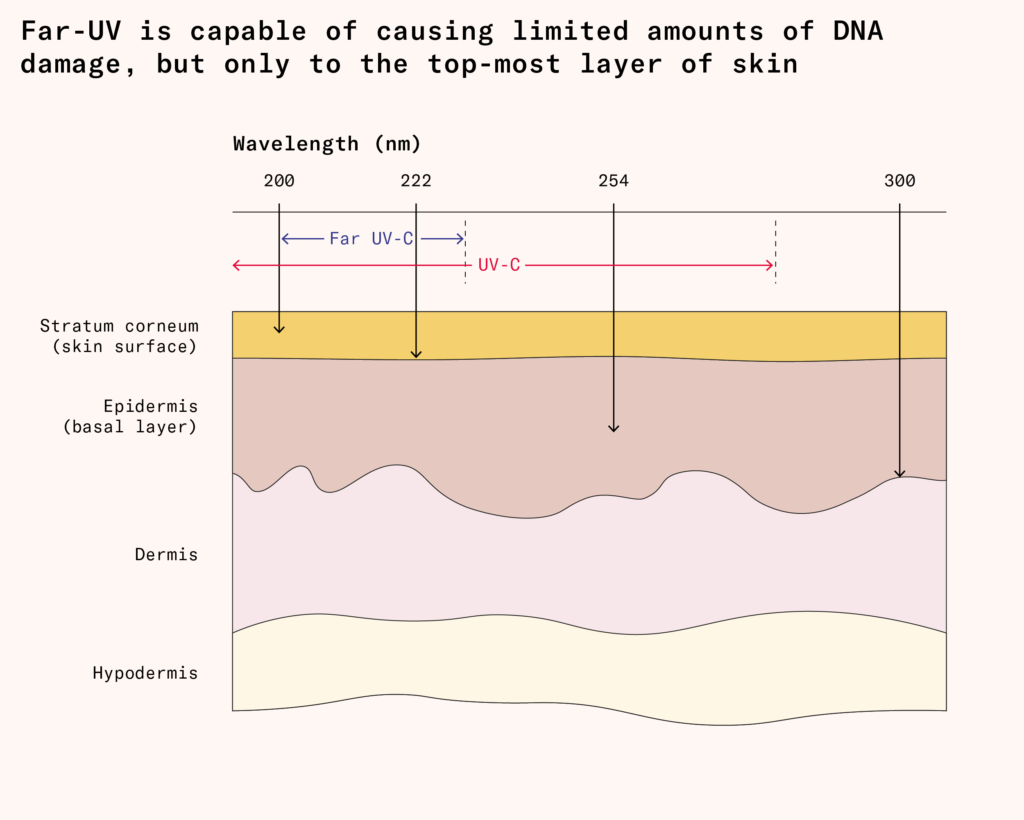
Just as filtration and chlorination made drinking water safe at scale, we now have the tools to do the same for indoor air: ventilation, high-quality filters, and germicidal light. A century ago, germicidal light at 254 nanometers seemed to be a promising way of controlling pathogens by killing them in the air, but it turned out to cause irritation and cancer in the skin, and it was largely dropped when antibiotics became widespread.
But today there is an update that has none of these drawbacks. We now know that wavelengths under 230 nanometers, especially 222 nanometer light, are harmless to humans, but can still disable microscopic pathogens. We know how to filter out all wavelengths except the ones we want, and how to direct them away from humans, cycling the air through them to clean it without exposing people to it, just in case it carries unknown risks. This far-UVC light, as it is called, may be how we can make the air we breathe as safe as the water we drink.
The sterilamp
Until the mid-nineteenth century, most physicians believed that disease spread through miasmas, poisonous vapors rising from filth and decay. Contemporaries were obsessed with air: moving to the countryside for the air, taking the air at the seaside. Bad air was blamed for sickness. Herbs were burned to purify the air to fight the plague. But because they didn’t understand what made the air dirty, they were not very good at cleaning it. This began to change only when Louis Pasteur and Robert Koch provided the first definitive proof that microscopic organisms were responsible for infectious disease.
Cleaning air relies on the same fundamental techniques as cleaning water: replacement, filtration, and disinfection. Pathogens replicate inside people, who then expel them into the air by breathing, talking, or coughing, where they can remain suspended and infect new individuals. The relative contributions of aerosol transmission, droplet transmission, and fomite (surface) transmission vary between diseases. Certain diseases, such as Covid-19, are driven by a small number of highly infectious individuals (‘superspreaders’) that account for a disproportionate number of cases.
In 1877, British researchers Arthur Downes and Thomas Blunt stumbled upon a discovery that would lay the groundwork for modern disinfection. In a paper submitted to the Royal Society of London, they described how over the course of six months they had used sunlight to prevent bacteria from growing in a tube.
Follow-up research by Robert Koch demonstrated that sunlight could kill Mycobacterium tuberculosis, but the early experiments lacked precision. Scientists knew light worked, but not which parts of the spectrum were responsible. The turning point came in 1930, when Frederick L Gates published the first quantitative analysis of how ultraviolet light affected bacteria, pinpointing peak germicidal effectiveness at 265 nanometers, the same point that nucleic acids – DNA and RNA – absorb light.
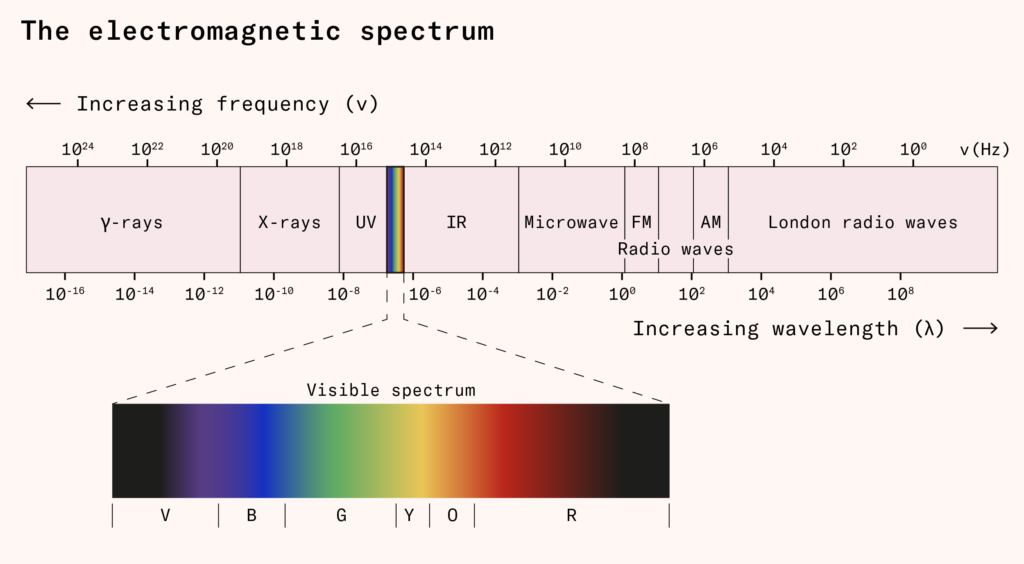
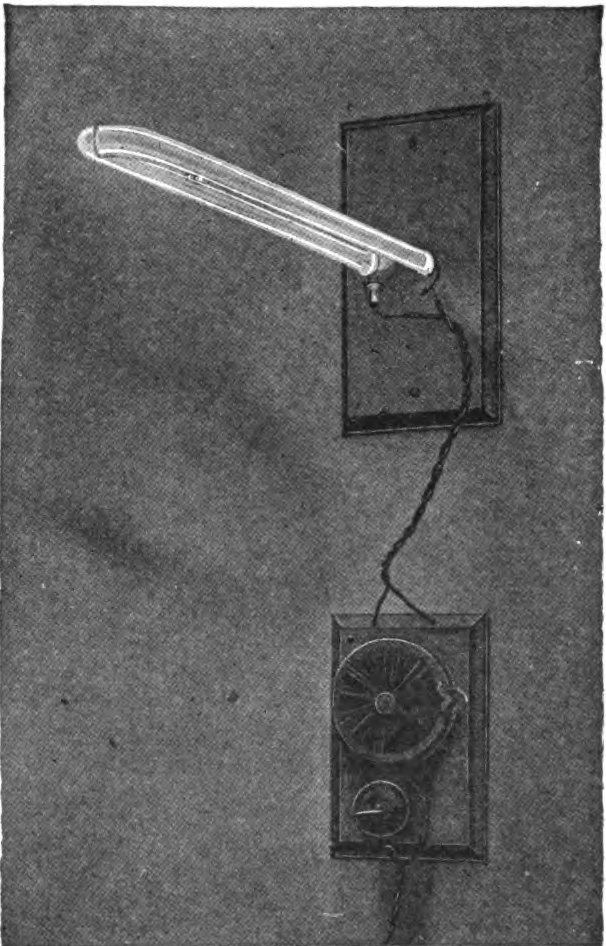
Understanding the spectrum wasn’t necessary for harnessing it. In 1901, American electrical engineer Peter Cooper Hewitt patented the first mercury-vapor lamp to achieve widespread commercial success. Hewitt created a voltage difference across electrodes in a glass tube, with mercury vapor causing electrons to separate from mercury atoms and collide with other atoms, exciting them to higher energy states. When these excited atoms return to their ground state, they release energy as photons, primarily at a wavelength of 254 nanometers.
Nucleic acids absorb this 254-nanometer light and produce new bonds between bases, preventing DNA/RNA replication. For human skin and eyes, this means sunburn-like irritation. But for viruses, amoeba, and bacteria in the air, as engineers at an American manufacturing company put it, these rays spell doom.
An array of different factors influences how sensitive pathogens are to ultraviolet-C (UVC), ultraviolet light with a wavelength of 100–280 nanometers. Viruses with larger genomes – such as herpesviruses (which have about 150,000 base pairs) or coronaviruses (30,000 base pairs) – offer many nucleotide bonds for photons to break, so they can be more quickly disabled than small-genome viruses such as parvoviruses (5,000 base pairs).
In 1936, Dr. Deryl Hart, a surgeon at Duke University Hospital, became the first person to use ultraviolet radiation to curb airborne infections in surgical operating rooms. High-intensity germicidal ultraviolet light fixtures, designed to irradiate the entire room, cut postoperative wound infection rates from 11.6 percent to just 0.2 percent, and not one patient out of 2,463 cases died from postoperative infections.
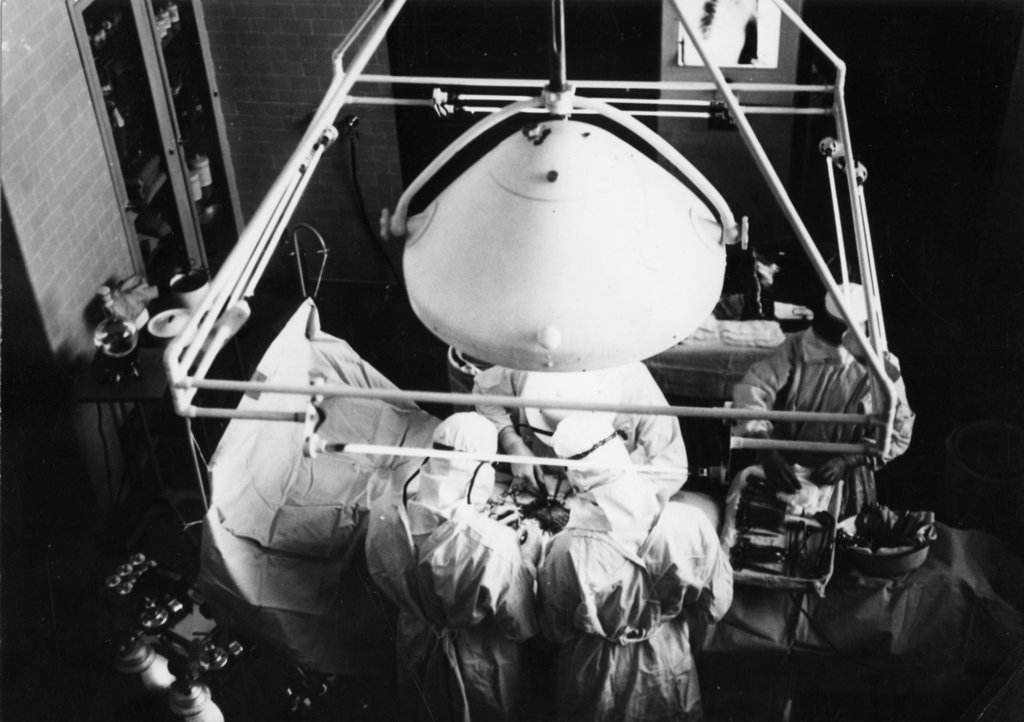
Shortly after the installation at Duke, UV from mercury vapor lamps was used to create invisible ‘curtains’ between cubicles in hospital wards and cribs in nurseries in Philadelphia, Boston, Toronto, and Evanston. In Boston, this attempt to prevent respiratory pathogens from crossing cubicles and infecting infant patients led to infection rates that were a quarter of those in the other cubicles. In the other cases, cross-infections fell by between 40 percent and 96 percent.
In 1937, researchers installed upper-room germicidal UV lights in the Germantown Friends School in Philadelphia and studied its impact over the next few school years. During the fourth year of the study, Philadelphia saw its largest recorded epidemic of measles, the most transmissible known pathogen. In the irradiated classrooms, only 14.5 percent of susceptible children fell ill, while in the unprotected ones, infection rates soared to 55 percent.

At the height of World War II, US defence manufacturer Westinghouse wrote that it was ‘fighting two wars at once’: one against the Germans and Japanese and the other against germs. Once a major producer of UV lamps and fixtures, the company had developed the Sterilamp in the 1930s. The Sterilamp system is described in a 1943 newsletter as a ‘DEATH RAY THAT GUARDS LIFE’.
But the deployment of germicidal UV light stalled after the war. In 1945–46, the New York Department of Health tried to replicate the Philadelphia findings in large public rural schools and failed. In one of the schools with an internal control group in Port Byron, 90.4 percent of susceptible students in UV-treated classrooms still contracted measles, compared to 83 percent in unirradiated classrooms.
Once they took bus ridership into account, the researchers found that UV had appeared to reduce the measles incidence rate by roughly 8.2 percentage points (from 77.4 percent to 69.2 percent) in non-bus riders. Germicidal UV could disrupt measles transmission in specific spaces such as classrooms, but it proved insufficient if face-to-face exposure continued in buses, hallways, and other shared spaces. Mercury lamps were also costly and could irritate the skin and eyes of people exposed to them. No long-term effects had been observed in humans at the doses used in schools, but higher doses had been shown to raise long-term cancer risk in mice. At the same time, the large-scale emergence of antibiotics was transforming the fight against infectious diseases. By 1945, mass production made penicillin widely available, ushering in the antibiotic era and shifting the medical focus toward drug-based infection control. Together with the failures of the UV studies, interest in germicidal UV receded.
Returning from obsolescence
Decades later, over 700,000 people a year die from antibiotic resistance as people use more and more antibiotics while their discovery rates stagnate. Airborne viral pandemics, which antibiotics cannot treat, have caused enormous economic damage and inflicted tens of millions of deaths. There is once again a case for the use of germicidal ultraviolet light.
Skin and eye irritation and cancer risks limited direct exposure to 254-nanometer germicidal UV to surgical cases. But new technologies – circulation, light filtering, and lower wavelengths – have together fixed these problems.
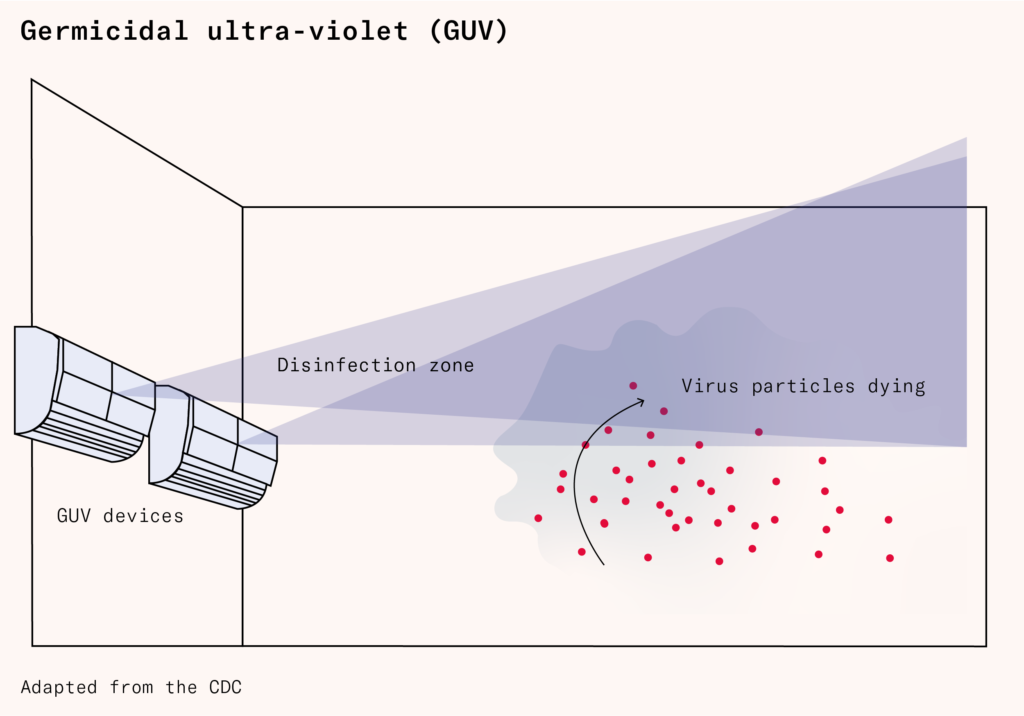
If we can circulate air, we can move it, clean it, and put it back. Today’s systems do this by projecting beams across the upper level of a room, above the heads of occupants. Natural circulation patterns move air to the ceiling, where it is cleaned, before it falls back down. But even reflected beams can cause irritation, meaning that each installation has to be calibrated carefully for the specifics of the room. Even repainting or shifting furniture can change the reflection of the beams, meaning that the UV beams would need to be recalibrated.
Shorter-wavelength light works just as effectively, without many of the downsides. Light with a wavelength of 230 nanometers or lower, known as ‘far-UVC’, disables pathogens without hurting humans, but mercury lamps cannot produce it.
Unlike longer wavelengths, far-UVC penetrates weakly, meaning it is only absorbed by the uppermost layers of the skin and eye, tissues which slough off frequently and do not divide. When shone directly into the eyes, germicidal doses of far-UVC do not appear to have any effect beyond temporary discomfort (the same as if a torch was shone into your eyes). When installed overhead, the lamp’s positioning and human facial structure mean only five percent of the light reaches the eye, creating an even larger safety margin.
Long-term exposure does not harm mice at all, even those with a severely limited ability to repair DNA defects. In humans, a 36-month-long trial installation of far-UVC in a hospital, with ongoing exposure to germicidal doses, caused no adverse effects on those working on the ward. There is no evidence from any other study that far-UVC raises cancer rates, though more work should be done to prove this beyond any doubt.
In order to prevent disease transmission, far-UVC lamps must disable pathogens in respiratory aerosols quickly enough that, by the time they are inhaled, not enough for an infectious dose remain.
A 2024 study presented some of the best data on far-UVC in an occupied room. Four lamps were installed in a lab mouse cage-cleaning room, where the constant activity and movement continuously aerosolized murine norovirus present in the bedding. When switched on, the lamps reduced the amount of virus in the air by 98 percent, equivalent to at least 36 air changes per hour. This happened despite murine norovirus being more resistant to far-UVC than many common human respiratory viruses, likely due to its tough protein outer ‘shell’.
Alternatives
There are other ways to clean the air, like ventilation and filtration. There’s an important role for both of these approaches, but they come with critical limitations that only far-UVC can plausibly overcome.
Ventilation is the easiest method of removing things from indoor air, diluting pathogens and pollutants into the 5.5 quadrillion tonnes of atmosphere outside. But it is not always convenient. It can be awkward or noisy to install and run. In highly polluted areas, bringing in outdoor air reduces disease transmission at the expense of worse air quality. In 2024, only seven countries met World Health Organization air quality standards. In very hot or cold places, outdoor air must be heated or cooled, which can be energy-intensive and costly, especially in older or heritage buildings where air conditioning needs to be retrofitted.
Another technique is filtration. Mechanical filters work by forcing air through a dense, pleated mesh of fine fibers that trap hazardous particles. Originally developed as part of the Manhattan Project to prevent the spread of radioactive particles, mechanical filters have become standard in hospitals, cleanrooms, and aircraft cabins.
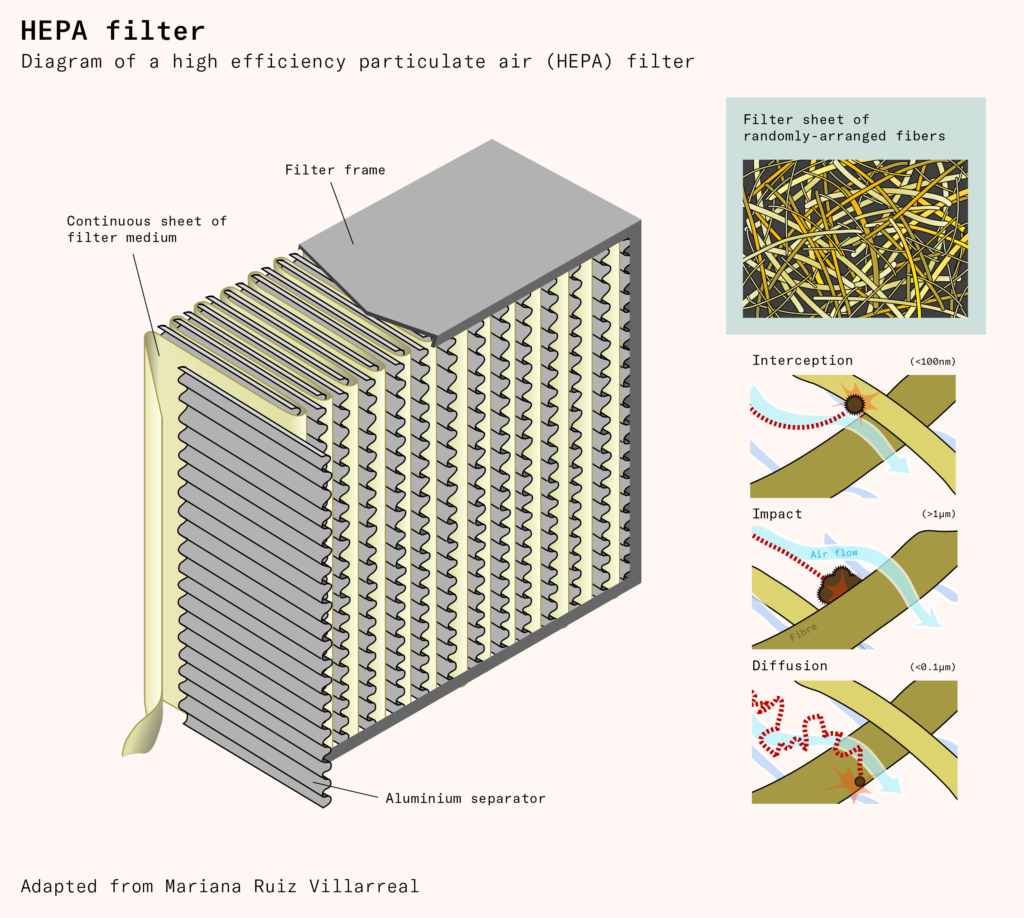
Mechanical filters are ‘plug and play’: there are dozens of verified and recommended models that anyone can buy off the shelf, install in their house by plugging them in, and expect to deliver reduced pollutants, allergens, and cleaner air for between $80 and $300. Consumer far-UVC systems are often considerably more expensive – a typical example costs $2,500 for a lamp covering 1,000 square feet, although a newer model has recently come to market at $600, and less expensive lamps with lower output can be added together to cover a similar floorspace.
The drawbacks of ventilation-based air filtration methods are similar to the drawbacks of ventilation itself. Moving air from place to place and forcing it through a fine filter requires energy, and fresh air from outdoors is often at the wrong temperature, requiring extra heating or cooling. Meanwhile, the constant air movement can also chill the air to the point of discomfort, requiring indoor heating. This has obvious impacts on the costs and environmental footprint of buildings.
Doubling the ventilation rate from the US standard minimum in offices could add up to $40 per person per year to building running costs. This is lower than typically predicted, but still more than double what many building officials were prepared (before the pandemic) to pay. Energy recovery units help equalize the temperatures between intake and exhaust air, and can lower these figures by about 60 percent (or even more), depending on local climate and system type. However, in Europe, the hurdle is even higher: most buildings have no mechanical ventilation at all, so adapting existing ventilation systems is out of the question. For example, in the UK, an engineering review found that only five percent of residential buildings were likely to have air conditioning (a proxy for mechanical ventilation) by 2019. By contrast, in the US, about 90 percent of residences have air conditioning.
Ventilation comes with another tradeoff: noise. The more air you filter, the harder your fan has to work, the faster it spins, and the louder it gets. Free-standing filtration units can be powerful, quiet, or affordable – but rarely all three at once. Purpose-built ventilation can be made quieter, but quiet movement of a large volume of air requires wide, leak-free ducting, which can increase installation complexity. Real world studies have shown that the noise and discomfort created by even relatively modest free-standing units mean that they are frequently turned down or switched off.
These drawbacks mean that ventilation-based methods lack the power to effectively block transmission of highly infectious pathogens or prevent pandemics. Without UV light, public buildings will require air handling systems akin to those in hospital isolation rooms to comply with current infection control guidelines. While circumstances vary from place to place, ventilation-based air quality measures quickly become impractical beyond around five air changes per hour, while upper-room UV light can achieve the equivalent of 35 air changes per hour, and far-UVC has the potential to reach well over 100.
Despite this, both ventilation and filtration need to be kept in mind as new buildings replace the old. If nothing else, ventilation design is an important factor in determining the effectiveness of UV systems; how well air is mixed and how quickly it moves affects the degree to which pathogens are exposed to UV light. These interactions have a positive or negative effect on pathogen removal. We flush and filter water, but we also disinfect it to eliminate remaining microbes. Air should be treated no differently.
Far-UVC is like an aerial disinfectant or bleach, except that it is harmless to humans at practical germicidal doses, and thus should not provoke resistance to its uptake. It does not alter pathogens in a way that allows resistance to emerge, a serious problem for antibiotics. Instead, it thoroughly damages microbial genomes at random, destroying bacteria and viruses alike, whether they are drug-resistant, vaccine-evasive, or indeed newly emerged.
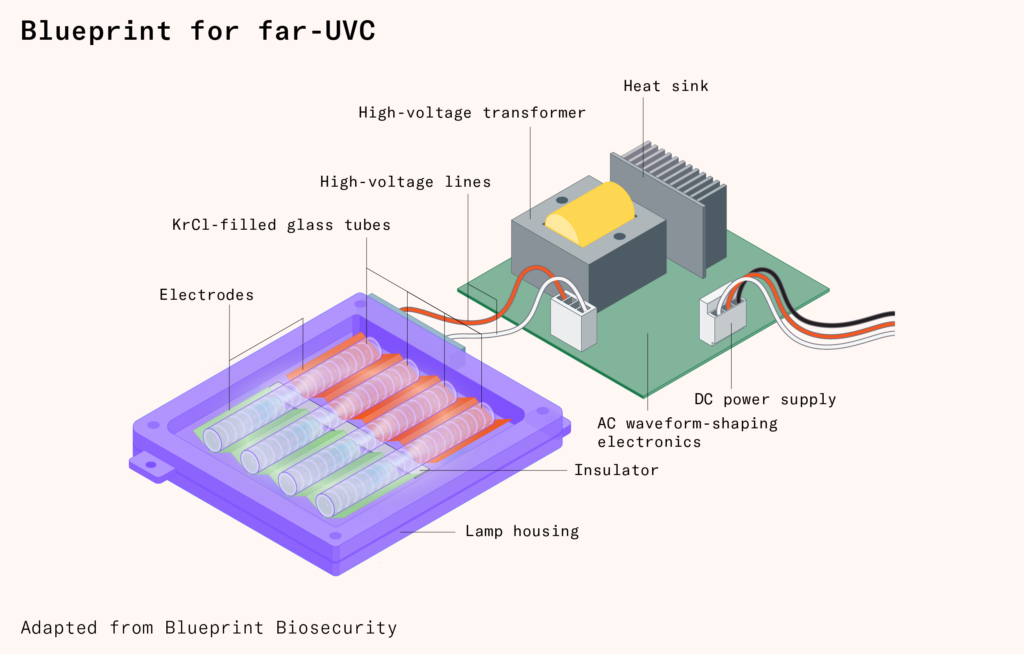
The most widely used commercial far-UVC source is a krypton-chloride excimer lamp. ‘Excimer’ is a contraction of ‘excited dimer’, a short-lived, high-energy molecule formed when the krypton and chlorine temporarily bond in an excited state as an electric current is passed through the gas mixture.
Krypton chloride lamps emit mostly 222-nanometer light, produced by the excited dimer decaying to its ground state and releasing the excess energy as a photon. Light at this wavelength is safe for human eyes and skin at doses that efficiently kill germs, but about 10–20 percent of the output consists of longer wavelengths with much lower maximum exposures. To use the lamps in occupied spaces, a filter with multiple layers of quartz and hafnium oxide is used to reflect unwanted wavelengths while allowing 222-nanometer light through.
Despite its potential, far-UVC has yet to achieve widespread use.
The very best krypton chloride emitters on the market are reliable, long-lasting, powerful, use little energy, and come with effective optical filters. But the state of the art is not representative. The krypton-chloride lamp industry is plagued by low-quality products with short lifespans that may not even produce any far-UVC light, and could even emit dangerous longer wavelengths. There is no product standard certification for UV lamps.
Top-tier excimer lamps, from reputable manufacturers, are expensive. This is partly due to their inherent complexity but largely from sluggish demand. The key reason is that, notwithstanding their successes in the 1930s, a certification vacuum denies buyers an authoritative seal of efficacy.
In part, this is because some of the studies establishing far-UVC’s efficacy aren’t as definitive as they need to be to really move the dial. One study on the impact of germicidal UV installations on tuberculosis transmission in homeless shelters was unsuccessful when the national rate of tuberculosis declined, which meant that the study ended up being too small to detect an effect even in principle.
In another study, germicidal UV was installed in hospitals to assess the impact of germicidal UV on flu transmission, but during the course of that study, the hospitals stopped routine flu testing. In a classroom study, not all classrooms had enough electrical sockets to plug in the portable air cleaners required for the study, some teachers turned off the air filters because they were too loud, and some schools didn’t install the germicidal UV devices they were supposed to because there were no legal protections for them for doing so.
But there are many other factors as well. Measuring infection control is challenging and seldom undertaken, particularly in public spaces. Epidemiological data is expensive and difficult to gather, and there is currently no way to measure the amount of viable, infectious pathogens in the air in real time. Office attendance can be tracked, but controlling for how users mix outside the office space is immensely difficult, and measuring the real-world effect of small-scale deployments in public areas is almost impossible. Studies aiming to cause deliberate disease transmission in controlled environments have failed to work in practice because they have been too small to generate enough infections.
Pathogen-free air and the research that goes into getting it are both, to some extent, public goods: the beneficiaries will mostly be people who haven’t paid for them. Even if a business reduces pathogens in its offices’ air, the biggest upside goes to other people who share spaces with its employees. This could be commuters on the same train, people in shops, or parents whose children attend the same school.
Despite the lack of clear economic upside, we are already seeing some early adoption among respected institutions: Mount Sinai Hospital, for example, has far-UVC lamps installed in its Cohen Center for Recovery from Complex Chronic Illnesses. Ideally, others would emulate this example, creating a stronger basis for research.
If one part of the knot were cut, then one of the most promising disease-fighting technologies of our time could finally be employed en masse.
In the early 1900s, a public health official in Jersey City, John Leal, lost his father to illness likely caused by contaminated drinking water.
But Leal had an opportunity to prevent such a loss for others: he quietly directed the addition of chlorine to the drinking water supply in Jersey City, hiring engineer George Fuller to design and build a system for dripping a diluted bleach solution into Boonton Reservoir. He believed that this common household bleach agent could kill pathogens without harming people. He was right.
Beyond being a triumph of science, water sanitation led to a fundamental shift in public expectations. Once people saw that clean water was possible, they demanded it.
Twentieth-century water treatment programs transformed public health by virtually eliminating waterborne diseases. Ventilation, filtration and disinfection provide us with the opportunity to dramatically reduce the burden of airborne illnesses. Tuberculosis and coronaviruses would join typhoid and cholera as tragedies of the past, and seasonal flu and common colds would become rare rather than routine if clean air were as universal and expected as clean water.
